What is a QIP?
So you’re thinking of doing a QIP, what next?
Quality improvement is the framework used to systematically improve processes and systems, particularly in healthcare and medical systems. Quality improvement (QI) aims to make a difference to patient safety and the effectiveness and experience of care, through using our understanding of the complex healthcare environment, applying a systematic approach to issues identified and designing, implementing and testing changes using cyclical processes to measure improvements.QI is comprised of tools, techniques and frameworks for systematically improving processes and systems, but where human factors are involved, should also account for shifts in mindsets and organisational culture. It allows organisations to continually work towards improving the quality of care by showing them where and how they might be falling short so they can implement measures to mitigate or improve this.
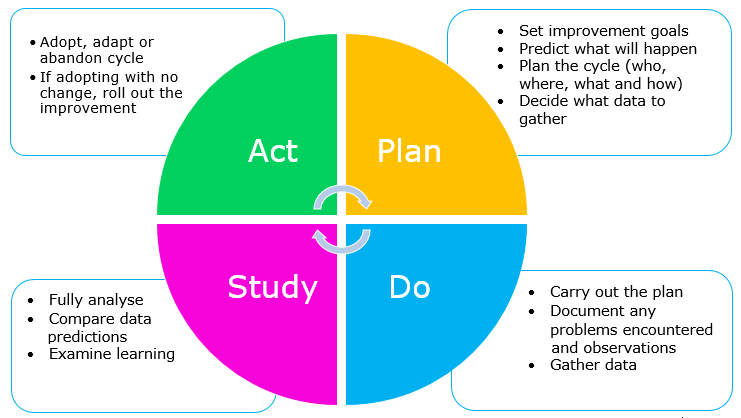
Audits are a very similar process, however have a more formal standard to measure against, for example a NICE guideline criteria, and may also tend to have a longer time period, for example once every few months rather than weekly/daily. QI can be done using the plan, do, study, act (PDSA) framework [Figure 1] with iterative cycles, allowing improvement to be incorporated quickly. Furthermore, QI can focus on holistic issues, such as patient perceptions.They form one of the 7 pillars of clinical governance. Quality improvement projects (QIPs) or audits are often part of standardised requirements for progression in training and make up sections of training and portfolio applications, signifying their importance to the NHS.
Why are they important and what can I achieve by doing one?
QIPs are important for a number of reasons.
- They let you impact and improve patient care as a junior doctor
- They allow you to gain a better understanding of issues surrounding patient care and strategies to improve these
- Allows you to address concerns about the way care processes and systems are developed
- You will develop a better ability to manage complex situations and problems, and will gain training and insight into human factors and how these impact the healthcare environment
- QIPs allow for gaining a better understanding of clinical governance and processes required to influence and positively impact care
- You can develop transferable skills such as leadership, time management and teamwork
- They can be presented at conferences, or written up for publication
- They count towards your ARCP requirements, but can also count for points for training applications
Even if you are a medical student, undertaking audits and quality improvement projects can be extremely useful either as first steps in a research journey or to gain a better understanding of the healthcare system and processes. Whilst it may also allow you to contribute to your portfolio as a student, it is important to be aware that some portfolios will specify a time limit in which the audit/QIP should have been completed, so you should be careful of this too. Certain SFP (specialised foundation programme) deaneries such as Yorkshire and The Humber, have now also started to utilise audit/QIP in their scoring matrix, so if aspiring to a career in clinical academia this can be a useful step.
How can I maximise the impact of my QIP?
Whilst most people will stop at simply doing a QIP, there are a few steps you can take to ensure you make the most of your hard work.
The process of starting an audit or QIP is to recruit your team, identifying relevant colleagues, and approaching the clinical governance department to register the audit/QIP after identifying a clinical problem. After collecting and evaluating data, you should follow the PDSA cycle implementing interventions and reauditing the change or the impact following your intervention.
With regards to ensuring you gain the maximum benefit for your portfolio there are a few things to be aware of – firstly, certain portfolios such as IMT now require a QIPAT form so it is worth looking into this beforehand to understand what formal processes or pieces of information you may need to undertake or collect. Secondly, portfolios can be quite specific with regards to the points allocated for different numbers of cycles – this is again worth checking to ensure you repeat the QIP/audit process enough times to gain maximal points, and is also worth thinking about when choosing a topic for example choosing one that is easy to repeat.
Another way to maximise the impact of your QIP is to present or publish your work. Particularly if you do multiple audits or QIPs through the course of your training, you can use some of these to gain publication or presentation points in your portfolio. If you conduct appropriate statistics in your reaudit process, looking at the difference or doing a t-test for example, and write up a structured abstract you can easily submit this to a conference in the speciality in which the audit is based, particularly if you have demonstrated a change or improvement. For example, my first ever national poster presentation at the Royal Society of Medicine was based on a GP-based QIP I conducted of prescribing in overactive bladder and adherence to prescribing pathways, discussing how we improved this with our audit cycle. Similarly, if over a long enough time period and with a significant enough change demonstrated, the results could be publishable – it may be worth liaising with a clinical academic in the same department to find out more about this.
To summarise, audits and QIPs can be a useful tool not only for personal and professional development but can also be a very valuable way to maximise your portfolios and progression.
